Patient Safety: It’s more than checking boxes
Making checklists work: KershawHealth excels as South Carolina experiments with surgical checklists
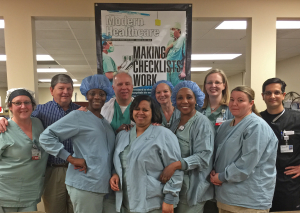 KershawHealth, Capella’s newest hospital, was featured on the cover of Modern Healthcare magazine the week of January 25, a result of the outstanding work they’ve done to improve care through use of surgical checklists. Their success has come through a two-year process, in association with a South Carolina Hospital Association initiative to get every hospital in the state to regularly use a pre-surgical safety checklist process.
KershawHealth, Capella’s newest hospital, was featured on the cover of Modern Healthcare magazine the week of January 25, a result of the outstanding work they’ve done to improve care through use of surgical checklists. Their success has come through a two-year process, in association with a South Carolina Hospital Association initiative to get every hospital in the state to regularly use a pre-surgical safety checklist process.
The new process requires that before any surgical procedure starts, everyone reviews the “KershawHealth Safe Surgery Checklist,” on the wall at the foot of the surgical table.
The surgical team reviews every item on the list prior to every surgery – out loud – with each member participating. The registered nurse confirms the patient’s name and date of birth, that X-ray equipment is in the room, and what allergies, if any, the patient has. The anesthesiologist states the type of drug being administered and whether there are any issues with the airway. The surgical technician, circulating nurse and others also weigh in.
Finally, the surgeon confirms the type of surgery, the anticipated time required, and notes whether or not the patient has any chronic health problems – such as diabetes or hypertension – that could affect the procedure’s outcome. The process concludes with an opportunity for any caregiver to speak up about anything else they believe needs to be contributed. The process lasts about two minutes.
The pause for the checklist is intended to help the team avoid terrible mistakes like operating on the wrong person or body part. It also facilitates communication among clinicians, who – historically at most hospitals – say surprisingly little to one another before, during or after a procedure. When used effectively, proponents say checklists improve efficiency in the OR, an area considered by some safety leaders to be among the most chaotic places in a hospital.
Surgical checklists, an approach drawn from commercial aviation and other high-risk industries, gained popularity when the World Health Organizatio n promoted them in 2007 under the leadership of surgeon and author Dr. Atul Gawande. He further popularized them in an influential book, The Checklist Manifesto, published in 2009.
Unfortunately, since that time, they have yet to become widely or systematically adopted. As a result, there’s not much data on their effectiveness, which in turn complicates further adoption.
South Carolina is now the testing ground for this more focused approach. In 2013, the South Carolina Hospital Association, working with Dr. Gawande and the Harvard University School of Public Health, launched a structured initiative to get every hospital in the state to regularly use a pre-surgical safety checklist process. The leaders of the project estimated that doing so could save 500 patient lives a year by averting medical mistakes. Harvard researchers gathered administrative data and data from the state’s death registry to track mortality outcomes in places that have adopted checklists. Initial findings have been submitted for peer review and may be published this spring.
Checklists fail when they’re tossed into an environment that doesn’t fully support the effort or when the checklist approach isn’t tailored to match the organization’s needs and culture, Dr. Gawande has said.
“It takes leadership support at the top and enthusiasts on the frontline,” he said. “You need both, because enthusiasm dies on the vine without a system behind you.”
Indeed, the South Carolina Hospital Association found that acceptance of the checklist process varied from hospital to hospital, but those that had the most success had committed to following all of the steps needed to become high-reliability organizations—they offered leadership support, financial resources and cultivated staff members who were dedicated to the enterprise. They also allowed staff to customize the process.
Research had shown that many hospitals, including KershawHealth, thought their surgical units were already safe, even though surgeons could start a procedure without uttering a word to the team, and staffers were afraid to speak up when they knew something was wrong.
KershawHealth updated its checklist in 2014, and its approach quickly gained statewide recognition. The hospital’s custom pre-surgery checklist has more than 25 boxes. While that seems like a lot, the team is able to go through them quickly. The hospital’s process also includes a required post-surgery “debrief.” Again, all members of the surgical team have a speaking role. This time, specimen labels are read out loud to confirm their accuracy, and staff has a chance to speak up if a piece of equipment did not work properly.
The KershawHealth staff also added a final box to the checklist, which asks: “What could have been done to make this case safer or more efficient?” In addition, the hospital posted checklist reminders in prominent places. A checklist hangs in each OR, and its jumbo font is large enough for everyone to clearly see. Reminders about timeouts and debriefs are posted at the entrance and exit of each surgical suite.
The facility now has nearly 100% compliance, which is tracked through monthly assessments of how often the checklist process was skipped.
Content taken in part from article by Sabriya Rice, published in Modern Healthcare magazine, January 25, 2016.
